Inflammation of the gums (gum disease) is the sixth most common disease in the world, so by definition is a disease epidemic!
Stages of disease
Gingivitis
Inflammation of the gums, due to the build-up of bacteria between the gums and the teeth. The bacteria and their toxins in plaque and tar-tar induce an inflammatory reaction. Usually bleeding and red gums that are tender to brush are some signs of gingivitis.
Periodontitis
Periodontitis is a progressive disease of the gums that destroys underlying bone and ligaments that support the teeth. Gingivitis becomes periodontal disease when the bone is lost. Unlike gingivitis, periodontitis is difficult to stop or reverse and more aggressive treatment is required. The bone loss is caused by the immune reaction of the body to the pathogens(bacteria). It is the reaction /overreaction of the immune system to the bacteria that causes the bone loss and periodontal disease.
Everyone’s response is different. So one person can have excellent plaque control & have severe periodontal disease and another person poor plaque control (poor oral hygiene) and no periodontal disease. It can be done to genetic make-up or other risk factors that can make this disease worse.
There are 3 stages of periodontitis
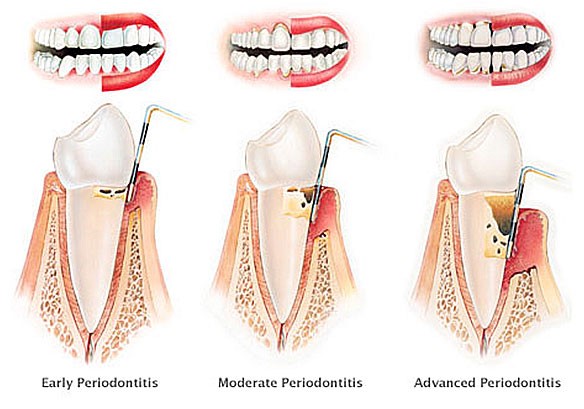
Early periodontitis: where few areas of the mouth have deep pockets more than 3 mm but less than 5mm


Moderate periodontitis: where most teeth have around 5 mm pockets and slight mobility of some teeth.

Severe/very severe periodontitis: where most teeth have 5mm+ pockets with great mobility and some furcation involvements/abcesses in the bone.
This case is classified as severe /very severe, generalized periodontitis, rapidly progressing with risk factors of genetics/smoking.

Periodontitis is usually painless. Therefore, our dental hygienist / therapist will assess and record your gum levels and monitor the health of your gums on a regular basis. Depending on the level of gum disease, some patients may require 3-month preventive care. Most health funds cover this service every six months.
In the case of periodontal disease, the only way to stop that disease from progressing, is the removal of calculus and debris from the root surface of the tooth – usually called root planning or deep cleaning which is usually performed under local anesthetic. The calcified deposits combined with biofilm (where the bacteria reside) must be removed so effective healing and homecare can be done.
Types of periodontal disease
New classification of gum disease (2017 world workshop)
Based on whether localized or generalized and staging and grading (very much like cancer diagnosis)
Location
Localized -if less than 1/3rd of teeth affected
Generalised -more than 1/3rd of dentition.
Affects just molars /incisors
Stage; amount of bone lost
Mild less than 15%, moderate1/3rd of bone lost,
Severe 2/3rd -2/3rd or
Very severe >2/3rds
Grade-slow, moderate or rapid for amount of bone loss /age
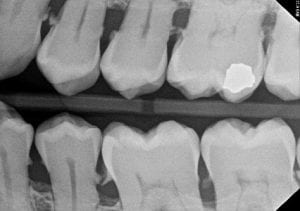
Can be uniform bone loss horizontally or vertical/ angular defect (sometimes called an infrabony pocket) seen below.

Perio-endo lesion
This is where there is periodontal disease and the nerve has died causing an area of infection in the gum and bone. Treatment requires root canal treatment as well as root debridement of the biofilm around the root. Luckily it can be saved in most cases, but requires more work& prognosis is not as good for this type of problem.

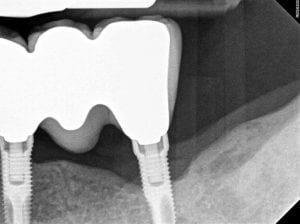
Peri-implantitis (gum disease in implants)
This is where there is periodontal disease and the nerve has died causing an area of infection in the gum and bone. Treatment requires root canal treatment as well as root debridement of the biofilm around the root. Luckily it can be saved in most cases but requires more work& prognosis is not as good for this type of problem.
Diagnosis of Periodontal Disease
This is done by the dentist /oral health therapist in conjunction with clinical examination, periodontal probing and radiographs.


Periodontal Analysis
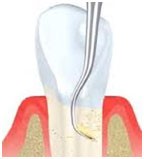
Periodontal analysis is where the dental professional measures the levels of both your gums and your bone using a special probe.
This process is usually performed on each patient, in order to assess the gum health and also acts as a base line for each patient.
The area between the tooth and the gums is called pockets. A healthy pocket is within 2-3mm. More than 3 mm is a sign of periodontal disease and more than 5mm would require deep cleaning/root planning.
Gum Disease Risk Assessment
Gum disease risk describes the likelihood of the health of your gums may worsen,(without professional intervention and appropriate homecare)resulting in inflammation /infection of your gums which can eventually lead to tooth loss.
Why Does This Matter?
Gum disease (periodontal disease) is the major cause of tooth loss in adults. Studies show long term retention of teeth improves overall general health & longevity. Gum disease is also linked to higher risk of heart disease, stroke, diabetes and rheumatoid arthritis.
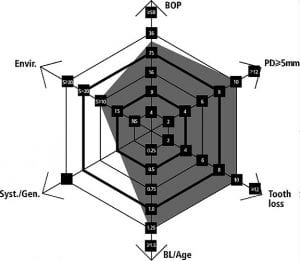
How do we do the risk assessment
Your dentist /oral health therapist will do this at the examination appointment when all the information is gathered. It is assessment of how active your disease is at present, pocket depths, environmental factors, medical issues, previous bone loss compared to your age.
The periodontal risk assessment or spider web diagram will pictorially show this and categorize into high, medium or low risk.
Example of high-risk periodontitis (gum disease)
Systemic risk factors
Genetics
There is genetic predisposition to certain types of aggressive gum disease.it is seen commonly in families where father or mother/siblings may suffer periodontal disease.it is important to identify this risk factor so appropriate prevention can be instituted.
Consider; checking family history if anyone has suffered with this, have you shared toothbrush and been inoculated by pathogenic bacteria.
Smoking
How is smoking related to gum disease?
Smoking reduces the body’s immune system to fight gum disease. The gum disease is more active, and the gums do not heal as well and recover from active infection.
As a smoker
Have twice the risk of gum disease compared to a nonsmoker? (increased pocket depth & bone loss)
The more cigarettes you smoke, the more risk of gum disease you have.
The longer you smoke the greater the risk of gum disease.
Treatment of gum disease does not work as well especially with surgical intervention.
Smoking of any kind of tobacco products; pipes, cigarettes, cigars, smokeless e- cigarettes carries the same risk, the nicotine having the effect on the gums.

Tobacco counselling; should you consider giving up smoking, our hygienist/therapist can discuss the different ways to quit. Alternatively, we can organize smoking cessation counselling through the hotline or we can refer to your GP.
Diabetes and oral health

What does diabetes have to do with gum disease?
People with diabetes have an increased risk of developing gum disease. Poorly managed blood sugar levels can cause damage to nerves, blood vessels, the heart, the kidneys, the eyes and the feet. In the same way, the gums can too be affected.
Because high blood sugar levels lead to damage to blood vessels, this reduces the supply of oxygen and nourishment to the gums, making infections of the gums and bones more likely.
Uncontrolled blood sugar levels can cause levels of glucose to rise in the saliva and this creates a breeding ground for bacteria, increasing the risk of gum disease and dental decay.
Severe gum disease can negatively affect your blood sugar control and increase your chances of suffering from other common long-term complications of diabetes. The inflammation, which occurs in the gums, escapes into the bloodstream and upsets the body’s defence system which in turn affects blood sugar control. In other words, gum disease and diabetes are linked in both directions.
Consider:
- Consult with your GP if your diabetes is not controlled well and referral to an endocrinologist.
- Active treatment of your gum disease; deep cleaning and follow up monitoring (supportive therapy)
- 3 monthly & Meticulous oral home care.
Medications that affect your gums
Enlarged gum tissue – overgrown or enlarged gum tissue is known as “gingival overgrowth” and is sometimes associated with antiseizure medications such as phenytoin, immunosuppressant drugs(cyclosporin) such as those taken after organ transplantations and calcium channel blockers(nifedipine, verapamil, amlodipine) that are taken by some heart patients to control blood pressure, anti-clotting medications (warfarin, aspirin)can cause excessive bleeding after gum treatments (deep cleaning) and especially if gum is lifted for a surgical approach for surgical debridement.

Please let your practitioner know what medications (including herbal meds) you are on & necessary advice/precautions taken.
The medications may worsen the gum disease so may need active treatment /surgery (removal of overgrowth) and more regular monitoring/supportive therapy.
Stress
It is now known that increased stress levels increase the risk of periodontal disease.it is thought to be due to the cortisol release and the body has less of an ability to fight infection also may effect standard of oral hygiene and other behaviors e.g. smoking.
Consider: reducing stress levels.
Bite and grinding/clenching.
A bad bite that has too much pressure on one tooth, or lack of back teeth can “overload” certain teeth and this can hasten the advancement of gum disease.
Consider: having a bad bite fixed by a dentist or get back teeth replaced so load is shared by entire dentition.
Also, there can be clenching and grinding that can overload several teeth and damage the supporting ligaments and bone.
Consider: occlusal splint to wear to prevent grinding.

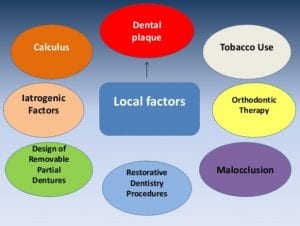
Local risk factors
These are risk factors located in the mouth that increase the risk of gum disease.
Overhanging margins and poorly contoured restorations
Poorly adapted/fitting restorations, ledges and open contacts can increase plaque retention & exacerbate gum disease. These need rectifying for the long-term reduction in gum disease levels.
Consider: these poorly fitting restorations need rectifying prior to /same time as gum treatments.


Partial Dentures
These prostheses encourage plaque accumulation around teeth that can make existing gum disease worse and lead to further tooth loss. the clasps on the denture can in effect wiggle the teeth loose if gum disease is active.

Consider: due to the higher risk of gum disease this requires more meticulous home care as well as regular hygiene visits to closely monitor gum disease levels. Ideally, elimination of the denture is better with the use of dental implant-supported /crowns and bridgework.
Crooked or malpositioned teeth
Crooked and mal-aligned teeth can make oral hygiene measures more difficult to keep clean, both brushing & interproximal care. see below plaque buildup and gingivitis on these malpositioned teeth that make hygiene a challenge.

Consider: braces or aligners to straighten teeth or spend extra time on home care so all surfaces are thoroughly cleaned.
Orthodontics/braces
This local factor can make cleaning a real challenge. the gum can react by increasing in size and become tender to brush. this is quite often seen in children with braces, however, adults can react by losing gum tissue and get recession if left untreated. see below active gingivitis and gingival overgrowth on upper especially.

Consider; improved oral hygiene using custom oral health aids to assist -eg platypus to floss under braces. Visit the hygienist more often for cleaning and help with methods to keep teeth as clean as possible.
Local tooth factors
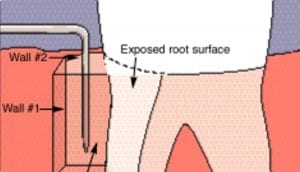
Presence of existing recession with exposure of grooves (furcation’s) on teeth roots can make oral hygiene a lot harder to perform. This places these teeth at higher risk of further gum disease and loss of bone. Below there has been a lot of previous recession exposing the roots and makes it extra difficult to clean in the molar regions where there is multiple roots.

Your personalised periodontal (gum disease) risk

Perio Risk
High, Medium, and Low depending on risk factors.
Treatment of periodontal disease
Routine scale & clean
This is the treatment of choice when the gum disease is mild, and the patient attends regularly with minimal tar -tar build up. A regular professional scale and clean is very important to achieve and maintain good oral health by removing plaque (soft, sticky bacteria, biofilm) and calculus (tartar) deposits that build on the teeth surfaces. Our therapist/hygienist will use special instruments to remove these deposits. Then correct oral home care is monitored, revised and updated to tailor the correct technique to keep the gum disease at bay. Usually every 3,6 or 12 months, depending on your gum disease risk for professional regular debridement (scale and clean), is required in the long-term maintenance. Our team will work with you to tailor the correct timeframe for review.
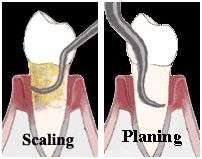
Reduce deep pockets with removal of biofilm and debridement of root-root planning (deep cleaning)
Usually our therapist/hygienist performs this procedure when there are pockets of 5mm, where calculus which harbor bacteria which is in a biofilm under the gums. Therefore, in order to prevent further attachment loss, the clinician will usually use special tools to go under the gums and remove all calculus from the root surfaces. This is done with an ultrasonic scaler which vibrates and dislodges the calcified plaque off and hand scalers that carefully clean the root surface. This procedure is usually done under local anesthetics or desensitization agents. follow up appointments are the key to success -normally 3 months. supportive ongoing care to monitor oral hygiene is done well will help maintain gum health.
Surgical treatment
This is where the gum is lifted up surgically, bone is smoothed and re-shaped and then sutured back. there can be more post-operative pain and swelling associated as well as significant costs increase.it is normally done when normal subgingival debridement has failed and no systemic risk factors.
Vertical bone defect
This is where the bone is lost in a vertical fashion. this indicates you may have an aggressive form or a localized anatomic issue that needs addressing.
Consider: Removal of toxins off the root under local anesthetic and application of antibiotics/systemic antibiotics if aggressive form of disease is diagnosed.
Raise gum surgically allowing access to area to clean thoroughly, then place stitches.
Surgically do the above & bone augmentation (graft) the area.
How long will treatment take to complete?
I expect that it will take up to four 45-60minute visits to complete this treatment, but it could be shorter or longer based on what we experience as the treatment progresses. It is important to success that 3 monthly supportive therapy is done to monitor gum condition & ensure correct oral hygiene measures are instituted.
Alternative treatment options:
- No treatment – there is high risk of pain, inflammation, abscess formation and tooth loss
- Offer referral to a specialist periodontist & the likely costs involved will significantly escalate
- Surgical treatment -lifting the gum up surgically and cleaning below the gum & removing any bony defects recontouring and suturing back the tissues. there is post-op pain, swelling and bleeding associated with this treatment and increased costs.
Risks of the recommended treatment:
Dental treatment is not completely risk-free. I will take reasonable steps to limit any complications of the treatment i have recommended. This is based on the individual circumstances of the patient, oral hygiene, medical history and social factors such as smoking and alcohol.
The complications that can occur during or after treatment which can contribute to a lower success rate or failure of treatment include:
- Post-operative pain/swelling or discomfort after treatment
- Continued infection of the gums (pus)
- Continued inflammation & bleeding, bone loss
- Sensitivity to cold air or fluids (due to debridement of roots & exposure of dentinal tubules)
- Loss of vitality & endodontic treatment down the track
- Further loss of bone /infection that leads to loss of the tooth
The success of gum disease treatment can be improved by following meticulous oral hygiene measures, keeping a low sugar diet, and stopping smoking and visiting the hygienist on a regular basis.
If you have any questions about these complications, or about any other complications you have heard or thought about, please ask. I believe that the treatment will be most successful when you understand as much as possible about it. No question is too simple to ask and I have as much time to answer them as you need.

